One Year In: How FM+ is Reshaping Primary Care in Manitoba
By Keir Johnson
One year after its launch, Family Medicine Plus (FM+) is making a measurable and meaningful impact on primary care in Manitoba. Introduced as part of the 2023 Physician Services Agreement, FM+ was designed to address the critical family doctor shortage, improve access to longitudinal care, and modernize Manitoba’s physician remuneration model to keep pace with other provinces.
Family Medicine Plus was officially launched on April 1, 2024, with a goal of supporting physicians who provide comprehensive, ongoing care to an attached panel of patients.
Dr. José François, a family physician who is now the Chief Medical Officer for Shared Health, explained that traditionally, “family doctors relied primarily on piecemeal funding for each patient visit, that sometimes left family doctors and patients feeling rushed.”
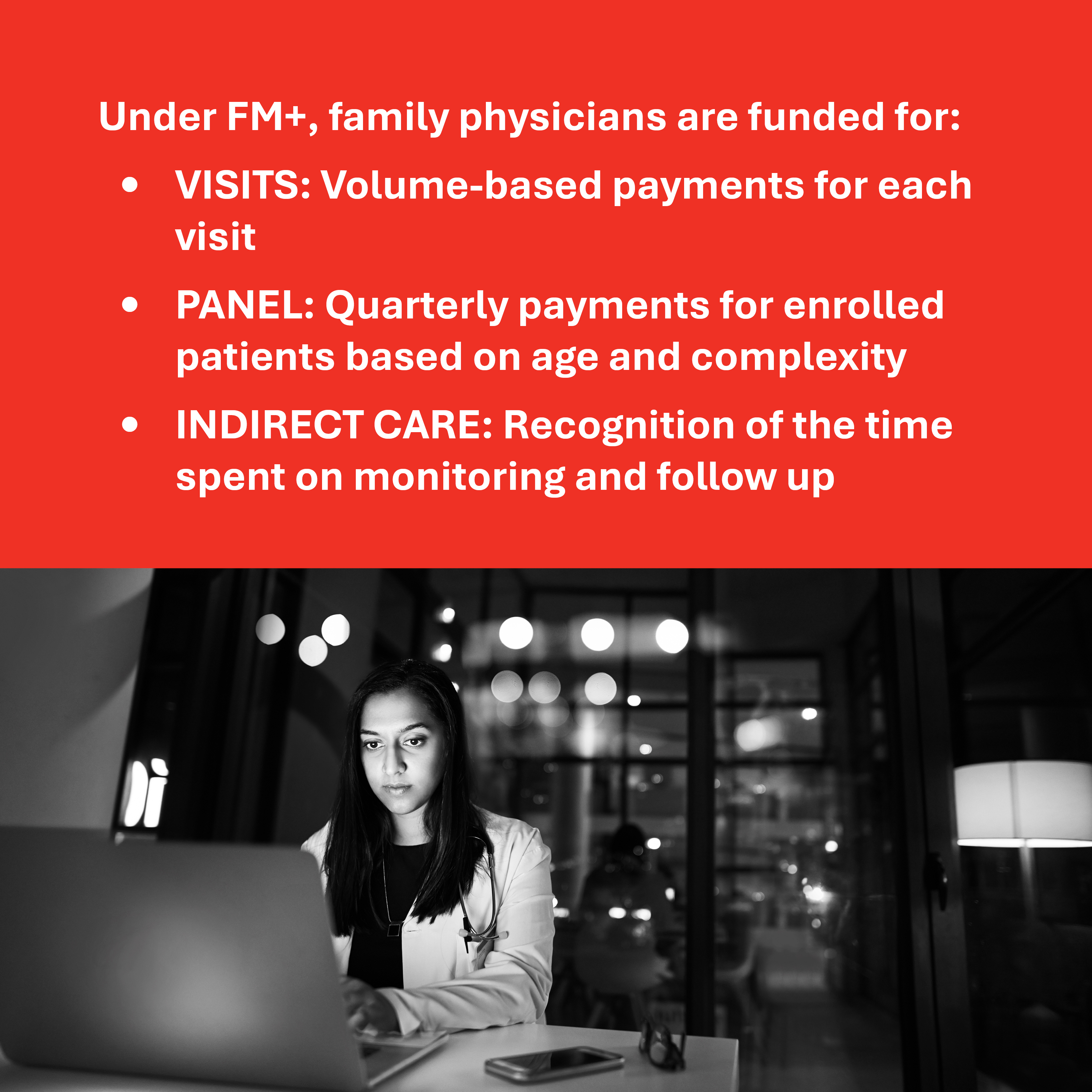
FM+ keeps the volume-based funding model, and complements it with stable funding based on the size of the patient panel a family physician carries, adjusted for age and complexity, while recognizing some of the time physicians spend on the monitoring and follow-up work that happens outside of the patient visit.
In other words, FM+ is designed to better support family physicians for the depth of care they provide — not just the number of services billed.
At the time of its introduction, FM+ was hailed as “a new era of family medicine” by Dr. Candace Bradshaw, a longitudinal family practice physician in Winnipeg who was also Past President of Doctors Manitoba at the time. “We call it FM+ because family medicine now means more in Manitoba.”
Family Medicine Department Head, Dr. Amanda Condon, explained at its launch that FM+ “is good for people with chronic conditions, as their family physicians are better supported to care for them.”
After a year of experience, however, it’s important to assess how FM+ is performing to ensure physicians and patients are both feeling a meaningful impact.
A Strong First Year
Doctors Manitoba undertook a preliminary evaluation to see how FM+ is performing after its first year in practice. The results are compelling:
- More doctors: There has been a net gain of 184 physicians practicing longitudinal family medicine, increasing from 654 to 838.
- More patients: There are 104,238 more patients attached to a family physician, bringing the total to over 1.025 million.
The initial analysis found participating family doctors have a healthy panel size of 990 patients on average. The model offers flexibility, recognizing some may practice longitudinal family practice part time as they offer hospital or episodic care part of the time as well.
There is no question that with core results like this, FM+ is improving Manitobans’ access to family physicians including improving the continuity of care.
While overall program costs are higher than anticipated due to its uptake and success, the per-physician cost is closely aligned with initial forecasts, suggesting strong program efficiency.
Physician Satisfaction is High
A recent survey of 445 participating family physicians found 84% were satisfied or very satisfied with FM+. Physicians cited several reasons:
- Recognition of the complexity and continuity of care they provide
- Fair compensation that is keeping up with other provinces
- Help managing rising overhead and operating costs
- Validation of indirect, non-billable work like paperwork, follow-ups, and patient coordination
Many physicians noted that the model made a tangible difference in their ability to stay in practice, expand their patient panels, or even reimagine their career paths.
- “FM+ is a gamechanger. I postponed retirement, feel less at risk of burnout, and it contributed to my willingness to accept new patients.”
- “This has allowed me to work rather than walking away.”
- “It certainly has incentivized adding more patients to my panel, especially newborns.”
- “Allows me to spend more time on my complicated patients without as much stress over financial compensation.”
- “Helps to validate the importance of longitudinal comprehensive care.”
A Shift in Culture
In addition to measurable outcomes, FM+ appears to be shifting the culture and morale of family medicine in the province. Many doctors emphasized how the model recognizes the unpaid, behind-the-scenes work that’s always been a part of good care — but never part of the payment model.
“I am no longer bitter about non-remunerated paperwork,” one physician noted in the evaluation.
Another added:
“I feel it recognizes the enormous amount of paperwork that accompanies having a family practice.”
Incentivizing True Primary Care
For decades, Manitoba’s primary care model was predominantly fee-for-service, with limited compensation for indirect care, following patients with complex needs, or attaching new patients. FM+ shifts this dynamic by rewarding continuity and comprehensiveness — what many physicians already view as core to family medicine.
“After 25 years in walk-in medicine, I made the switch,” explained Dr. Leslie Simard-Chiu. “I was seeing so many patients who couldn’t find a doctor because their needs were too complex. FM+ gave me the support I needed to make the leap. Yes, it’s been a ton of work — chart transfers, EMR adoption, late nights — but now I’m seeing the outcomes of my care, getting to know my patients, and feeling more motivated than ever.”
Physicians also reported improved continuity of care for patients, the ability to spend more time with those with complex needs, and reduced stress related to compensation and practice sustainability.
What’s Next?
Doctors Manitoba will continue to evaluate FM+ as it matures. The early results, however, strongly suggest that the model is helping to stabilize and grow Manitoba’s primary care capacity.
This progress is crucial, especially as other provinces roll out their own longitudinal payment models. FM+ ensures Manitoba is not only keeping up — but leading in valuing the work of family doctors and improving access to care for patients across the province.
A continued focus on FM+ couldn’t be more important considering Manitoba has the fewest family physicians per capita in Canada.
As Dr. Bradshaw explains, the new model returned hope to her professional life. “After years of chronic burnout, I feel the joy in practicing medicine again, knowing I’m spending more time with my patients and providing them with quality care.”