Beyond Sports
How musculoskeletal medicine supports high-performance living and an improved health care system
By Katiana Krawchenko
What keeps Dr. Hein Peters going is simple: seeing his patients move with less pain and more freedom. As a sport and exercise (SEM) physician at Winnipeg’s Pan Am Clinic, he finds deep satisfaction in helping people get back to the activities they love.
“It’s amazing to see,” said Dr. Peters. “And so satisfying.”
He’s helped athletes as the team physician for the Winnipeg Goldeyes for the past 15 years, but he is equally rewarded by his work caring for everyday Manitobans.
“For sure there are athletes but the majority of our patients are people that just want to stay active or have difficulty staying mobile,” said Dr. Peters, noting that he and his colleagues see a wide range of patients with sprains, strains, fractures and breaks, but also chronic degenerative conditions like osteoarthritis, tendonitis. “It is very rewarding to be able to help them.”
That’s a sentiment shared by his colleagues, whose main goal is to keep patients moving in order to get them back to the things they love to do. Once referred to as “sports medicine,” this form of musculoskeletal medicine is traditionally thought to be reserved for high-performing athletes, but that is far from reality, doctors say. These physicians are family doctors who have specialized training to diagnose, treat, and help prevent injuries surrounding bone, muscle or joint problems. The word “exercise” was added to the title to show that all are welcome and to dispel the notion for both referring colleagues and patients alike that SEM physicians hold an exclusive pro-athlete patient roster. Quite the opposite, they hope to take pressure off of family physicians who regularly see patients with musculoskeletal problems while taking some of the load off of colleagues in orthopedics and other specialties.
SEM doctors work in conjunction with surgeons and physiotherapists to help develop the best treatment plans for their patients, which can include education on lifestyle changes, pain-reducing injections, as well as pre- and post- operative care.
This work can include:
- Diagnosing and managing acute, degenerative, and overuse joint and muscular problems.
- Prescribing exercise and physical activity for maintaining good health and to prevent and treat chronic medical conditions like high blood pressure, heart disease, diabetes, osteoarthritis and depression.
- Treating exercise-related medical problems such as concussion and asthma.
- Providing care for people of all ages in recreational, amateur, elite, and professional sports including pre-participation medical assessments, sporting event medical coverage, anti-doping, environmental issues, mental health, and treating athletes with disabilities.
- Prevention of injury and medical illness related to physical activity and sport.
Common problems treated include back pain, osteoarthritis, rotator cuff pain, and workplace injuries, with a panel of patients that includes people of all ages and abilities.
Doctors Manitoba Board Member and SEM physician Dr. Ashley Olson, of Legacy Sport Medicine clinic, explained that this type of musculoskeletal medicine is more all-encompassing than the name sometimes suggests.
“The main part of the medicine that we want to practice is helping people get back to what they do and that involves so many components, especially through education and reassurance to the patients that we can keep them going and try to shift the way that they see themselves,” said Dr. Olson. “I’m often talking to people who are telling me ‘I’m not able to walk. I’m not able to play with my kids or grandkids.’ And that’s where I think our expertise really comes in from a physiological perspective and then a functional and occupational perspective. We’re all about restoring function and quality of life.”
By treating patients through prescriptions for exercise, education on lifestyle choices, braces, injections, and other therapies, SEM physicians can help reduce pain and thus decrease the use of oral painkillers while increasing quality of life.
“A lot of the time you see people who say, ‘well, my knee’s bummed, so I can’t walk. So then I’m gaining weight and my blood pressure goes up and my diabetes gets worse and now I have cardiovascular issues and I get depressed because I’m not getting out as much as I used to in my social circle,” explained Dr. Chris Morrow, who practices at Legacy Sport Medicine clinic in Winnipeg and also provides care to patients in Thompson.
Long wait times
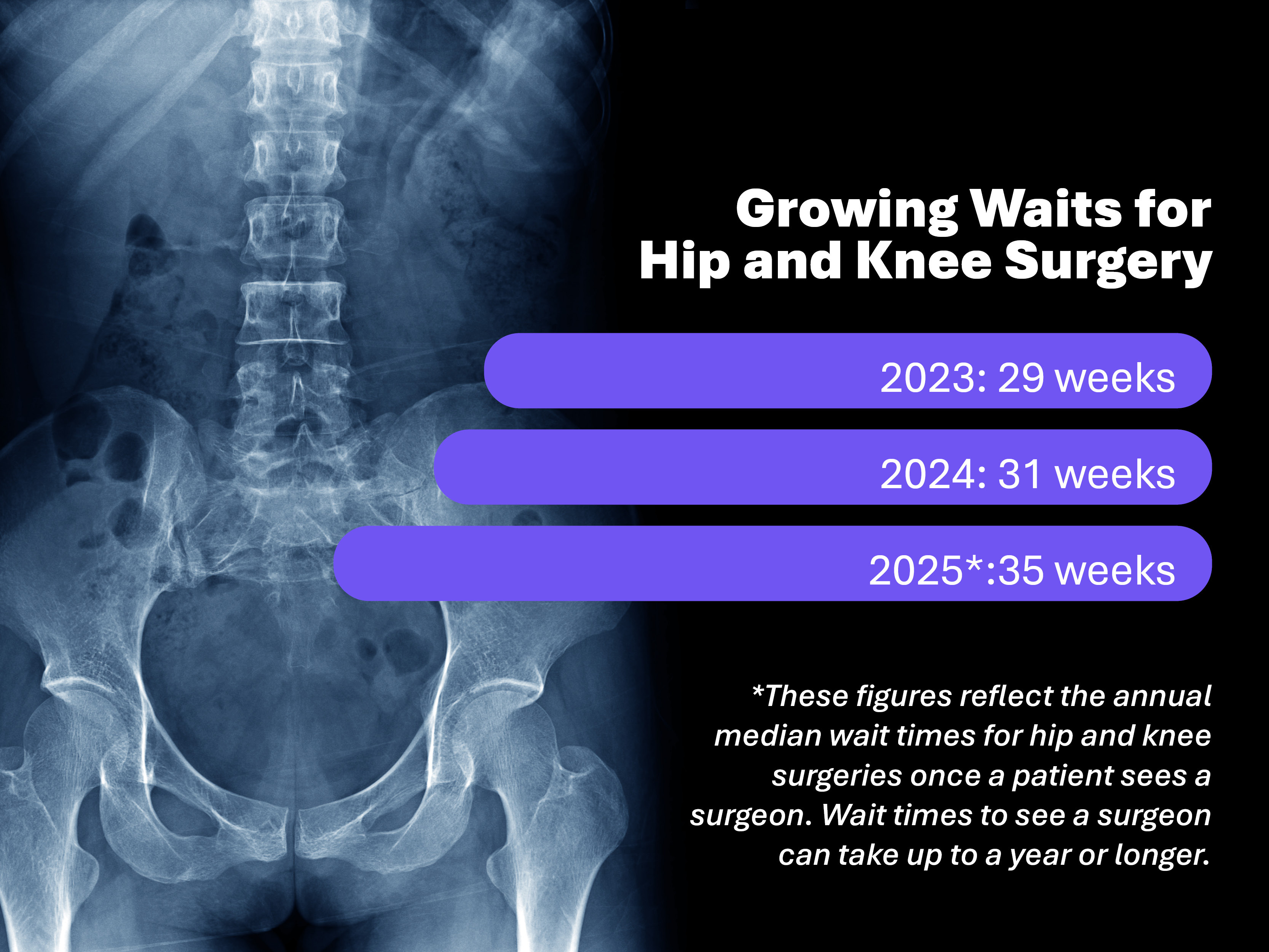
In Manitoba, it is not uncommon to spend several years on a waiting list for hip, knee, shoulder, spine, rotator cuff and ankle surgeries. “You can really see this downward trajectory,” he added. “We have this opportunity to intervene and take care of people. We can help you live your life.”
The care SEM physicians provide can help ease patients’ pain in that time and lead to better surgery outcomes.
“We know that keeping patients active, physically moving and physically strong is the number one predictor of success post-operatively,” Dr. Olson said. “And it also, of course, improves their quality of life while they’re waiting for surgery. It feels for some of them like a never-ending wait.”
Dr. Olson noted that many patients referred for joint replacement experience substantial symptom relief through optimized non-operative management, leading them to defer — and in some cases forgo — joint replacement.
She recalled one patient with advanced hip osteoarthritis who had been awaiting surgery, but was growing increasingly concerned that her worsening pain was affecting not only her quality of life, but also her ability to care for her husband and for them to remain in their home.
“She was understandably worried about her limited mobility and function leading up to surgery, as well as the expected demands of post-op recovery. We explored non-surgical options, including ultrasound-guided injections. Her pain and function improved to the extent that she and her surgeon mutually agreed to defer the hip replacement, indefinitely. She’s now more physically active than she has been in over a decade, has lost nearly 50 pounds, and is able to maintain her independence at home with her husband — outcomes that were highly meaningful to her, and certainly beneficial for her overall physical and mental wellbeing.”
Making Manitoba’s health system more efficient
The doctors agree that more referrals to, and investment in, musculoskeletal medicine can yield tremendous benefits for both patients and the healthcare system overall.
In Thompson and other Northern communities in particular, sport and exercise medicine can play a key role in not only reducing patients’ pain and discomfort, but also in making more efficient use of health resources that already run sparse.
“I was seeing GI bleeds from people taking too many oral anti-inflammatories and having to medevac them down to Winnipeg,” said Dr. Morrow, noting that having the ability to treat conditions through injections and movement rather than managing pain through addictive opiates has a hugely positive impact across the entire province.
“There’s this really simple solution,” said Dr. Morrow. “Treat the pain generator — the joint itself. If you can treat that well and keep the patient moving, then you’re solving a lot of different problems, like medevac-ing fewer people, there are fewer opiates in the community, there’s less addiction in the community. And then on top of that, you wouldn’t see this sort of downward spiral.”
Referrals
Musculoskeletal physicians encourage colleagues in family practice to send bone, joint and muscle issues their way.
“I hope that referring colleagues know that we’re here to support them as well,” said Dr. Olson. “If we can help offload the musculoskeletal pathology that we know is a huge component of primary care visits, we are here to do just that.”